MDMA is now proven to help those with trauma – so let’s decriminalise it and put it back in the medicine cabinet
A moral panic whipped up by the press in the 1980s led to ecstasy being banned. We owe it to those who suffer from alcoholism and PTSD to bring it back into use
When MDMA (later known as ecstasy) was discovered by Shulgin in the 1950s, he noted that it had very special properties of calmness, clarity and empathy that set it apart from the many other chemically related amphetamine-like drugs. He then told this to his wife, who was a psychotherapist and who agreed and suggested that these properties were ideal as a medicinal adjunct to psychotherapy.
She shared this knowledge and the drug to many therapists in the west coast of the US. They concurred with her analysis: MDMA was a real breakthrough in treatment, the first drug that could augment psychotherapy in which it was called “empathy”. It was especially useful in couples counselling where the empathy-enhancing effects could break down the years of tension and irritations with the partner that often build up in marriages and slowly crust over the early love and desires.
All was well until the MDMA was recruited by the rave scene as a “dance drug” and renamed ecstasy. This led to a backlash from the media who hated the idea of young people becoming ecstatic, and developed a campaign of moral panic to get it banned. Horror stories of brain damage were invented and the few deaths massively publicised in relation to the harms of MDMA compared with other drugs such as alcohol. This campaign worked and ecstasy was banned across the globe at the end of the 1980s, despite eloquent and compelling protestations from the many therapists that had used it and patients who had benefited.
MDMA is still illegal today despite the supposed scientific evidence of harm being largely discredited. Schedule 1 drug research with MDMA is hugely difficult and expansive but there is growing evidence of therapeutic value and neuroscience studies such as the new Gabay et al paper – reported in these pages – reveal that there is a strong scientific rationale behind its use.
A coalition of therapists in the US under the banner of the Multidisciplinary Association for Psychedelic Studies (Maps), has fought for more than 30 years to keep the therapeutic potential of MDMA alive. They have raised charitable funds to allow MDMA to be evaluated in its use treating people with resistant post-traumatic stress disorder. Several studies have been commissioned that cover both war and other causes of trauma, one taking place earlier this year. They show that just two psychotherapy sessions with MDMA as part of a psychological treatment course can massively improve PTSD – often resulting in a full recovery in patients who had to that point been resistant to other conventional forms of treatment such as the SSRI antidepressant medicines and cognitive behaviour therapy.
In light of these successes we have begun to treat people who have become alcohol dependent with MDMA in an attempt to deaden the mental pain of prior traumas. Such individuals are very common, indeed the norm, in alcohol treatment services and have a massively high failure rate with conventional abstinence-based treatments. Less than a quarter stay dry for three months, while those who carry on drinking for the rest of their lives have their life expectancy cut by 20 years. So far we have treated five people with the standard Maps protocol of two MDMA sessions two weeks apart, as part of the standard post-detox follow-up sessions. Up to this point all have stayed abstinent for the duration of the trial, which is still recruiting and will finally report next summer. We hope the early successes continue.
So how does a dance drug have such a powerful therapeutic effect? The answer, we believe, is because of its unique pharmacology that leads to its special psychological effects. MDMA releases serotonin, the neurotransmitter that we now know is involved in social bonding as well as in reducing anxiety and lifting depression. MDMA also releases dopamine, which is why it can be used to give energy for all night raves, but this is a secondary and lesser action. In the quiet of the therapeutic treatment room the dopamine release may help keep patients motivated and engaged with the therapist, but it’s the ability of the serotonin to overcome fear and anxiety that’s critical.
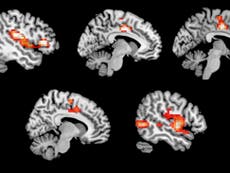
The current best treatment for PTSD involves reliving the trauma and gaining mastery over the emotions that emerge. For many severely traumatised individuals this is not easy: the memory can invoke such severe anxiety that the person can’t cope and leaves the room or they dissociate so can’t engage with the therapist. Our own brain-imaging study showed that MDMA dampens down the anxiety circuit of the brain and so reduces the impact of reliving negative memories.
This new study shows it enhances trust, which is vital in the therapeutic situation where the therapist is asking the patient to re-engage with memories they would rather forget. Together these neuroscientific advances give a firm rationale for the use of MDMA in PTSD therapy and support the call that I and many others have been making that it should be taken out of the controlled drugs list and put back into the medicine cabinet.
David Nutt is professor of neuropsychopharmacology at Imperial College London and chair of DrugScience.org



Join our commenting forum
Join thought-provoking conversations, follow other Independent readers and see their replies